Introduction
My former lab mates studied glycan physiology just before I started my freelance writing career. He studied mucosal glycans in the gut, where bacteria can use enzymes called glycoside hydrolases to use mucus as a nutrient source to facilitate gut colonization.
Our interview here is about glycans, but of the respiratory kind.
At SalivaDirect 25, I heard a captivating talk by Ravneet Grewal about how tobacco consumption affects respiratory glycans. As is the case in the gut with its intestinal lining, respiratory glycans protect our mouths and gums from dangerous pathogens that can wreak havoc in our bodies. But as you’ll see through this interview, tobacco smoking leaves patients even more vulnerable to infection and oral disease. And that’s not even considering what we already know about their links to cancer.
Read more about how tobacco smoking drives oral infectious diseases with mucin manipulation below!
The Interview
About Smoking
PN: For decades we’ve had debates about tobacco’s impact on our health. Now, the public seems to be well-aware of its dangers. What about tobacco is so dangerous to consume?
RG: Long-term tobacco use can harm nearly every organ, including the reproductive, digestive, nervous, respiratory, and cardiovascular systems. But tobacco is most dangerous in the oral cavity (mouth). People commonly consume tobacco by chewing it or smoking it.
Tobacco consumption is dangerous. It contains about 4000 chemical components, many of which are linked to cancer and toxic to consume. Starting and keeping the habit of smoking and chewing tobacco daily for years can lead to abnormalities and lesions in the oral mucosa. These abnormalities characterize various pathological conditions such as tobacco pouch lesions, precancerous conditions like leukoplakia, erythroplakia, and erythroleukoplakia, and cancers— squamous cell carcinoma and verrucous carcinoma.
About mucins
PN: Your research focuses on the effects of smoking on a major component of the saliva we produce in our mouths: mucins. What are they, and how do they boost our oral health?
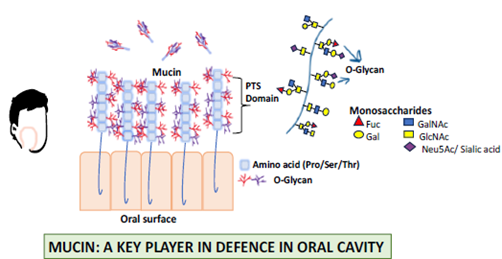
RG: Mucins are high-molecular-weight O-linked glycoproteins that are the primary structural components of mucus. The backbone comprises a sequence of amino acids, the building blocks of proteins. This sequence is enriched with cysteine residues that form disulfide bridges with other mucin monomers. N-acetylglucosamine (GlcNAc), N-acetylgalactosamine (GalNAc), fucose (Fuc), galactose (Gal), and sialic acid (Neu5Ac), build upon the peptide backbone, often with terminal sialic acid or fucose. When you combine the two components together, you form an extended brush-like structure at a molecular level. When glycan residues join, the mucins form a gel-like barrier in various bodily secretions that shields our oral tissues from damage and infection (Figure 1). That includes saliva, where they comprise ~26% of all salivary proteins.
PN: What happens when these mucin profiles are altered? Would it make us sicker?
RG: The primary function of mucin is to protect and repair the cell. They perform a wide range of other physiological functions as well. But an altered mucin profile, for instance, high levels of sialic acid, is like a friend turned into a foe. With this new avatar, they now promote an environment where an abnormal cell can easily escape the surveillance of our immune system, thus favouring a niche for cancer and other diseases.
About tobacco consumption and mucin glycosylation
PN: What are the mechanisms behind tobacco consumption contributing to aberrant mucin glycosylation profiles, and what are the consequences of these aberrant mucin profiles for our oral health?
RG: Consuming tobacco disrupts the very shield that protects our mouths from disease. Chronic tobacco use may also affect the machines that build our mucins. They can interfere with glycosyltransferases, enzymes that add sialic acid, fucose, or other glycan epitopes at the ends of mucins. How they affect other enzymes remains to be seen, but we know two things about long-term tobacco usage:
- Fewer mucins are secreted
- Terminal glycosylation undergoes aberrations
Both aspects can play significant roles in how oral diseases arise or progress in patients. Studying how tobacco usage impacts these enzymes could help us understand the molecular basis of any observed glycosylation changes in tobacco users.
PN: There are many kinds of tobacco in the world, and we even have alternatives to smoking such as vaping. Do any of these affect the risk of consuming tobacco?
RG: Yes, the type of tobacco product influences the severity of its adverse effects on oral mucosa, particularly mucin secretion in saliva. Our research has linked smokeless tobacco use to a greater reduction in mucin secretion compared to bidi smoking, likely due to the direct contact of harmful chemicals with the oral mucosa.
Smokeless tobacco products also have higher levels of various toxins, including tobacco-specific N-nitrosamines (TSNA), volatile N-nitrosamines, volatile aldehydes, polynuclear aromatic hydrocarbons, lactones, urethane, metals, radioactive polonium, and plant materials. That’s not to say bidi smoking isn’t toxic, either. Here’s some of the toxic compounds found in bidi smoking: carbon monoxide, hydrogen cyanide, benzene, 1,3-butadiene, substituted phenols, and o-xylene. Each of these toxins are linked to an increased risk of cancer and many other diseases. The worst part about bidi (a non-filtered cigarette) smoking is that far more toxins are present in it than cigarette smoking.
Vaping is expected to yield similar results, though the specific impact in terms of the adverse effects of chronic use on the oral mucosa needs investigation.
PN: You performed the study on secretory mucin glycosylation on a cohort from India. How universally do you anticipate these results across diverse ethnicities and peoples?
RG: Glycan diversification in complex multicellular organisms, including humans, is driven by a balance of endogenous and exogenous selection pressures. Exogenous selection, mediated by pathogens that recognize glycans, is believed to play a crucial role, favouring intra- and interspecies diversity. In humans, salivary mucins have multiple functions, including pathogen recognition. Terminal glycosylation of mucin is believed to undergo fine-tuning to keep pace with ever-evolving pathogenic pressures. This ongoing evolution of mucin glycosylation could influence the outcome in diverse populations.
When pathogens enter the mouth, they first interact with sialic acid or other glycans present at the ends of mucin. Interestingly, to counter the evolving nature of pathogens, the host modifies these glycans without impairing our health. It is conceivable that the survivors of a lethal disease might have some random glycan variations that likely protected them. These variations could be inherited, creating new population with glycan biology different from those who never encountered that pathogen. In that light, I expect different outcomes across diverse ethnicities and people.
Altogether, the glycans at the terminal position of mucin play a crucial role in pathogen recognition and defense in the oral cavity. They constantly evolve to adapt to new pathogens. This ongoing evolution of mucin glycosylation could influence how diverse ethnicities and people respond to long-term tobacco use.
PN: What are your plans to further explore aberrant glycosylation among tobacco smokers? What questions are you hoping to explore next and how are you hoping your data will help mitigate smoking and its effects on users?
RG: We performed this analysis with a small sample population. Now, when the impact of chronic tobacco use on mucin is established in the oral cavity, future investigation into a large sample population needs to be performed to warrant these novel findings. Further, I will focus on evaluating the behaviour of glycosyltransferases responsible for the decoration of sialic acid and fucose on the terminal ends of mucin in the saliva of tobacco users. This information will be crucial in developing effective interventions to address the health risks associated with tobacco use.
Author
-
Paul Naphtali is a seasoned online marketing consultant. He brings to the table three years of online marketing and copywriting experience within the life sciences industry. His MSc and PhD experience also provides him with the acumen to understand complex literature and translate it to any audience. This way, he can fulfill his passion for sharing the beauty of biomedical research and inspiring action from his readers.
View all posts